According to Moore’s dictum (newly minted by me, although I’ve had the idea for a long time), appropriate medical care must meet one of three criteria: either it makes us feel better, it makes us live longer, or it saves us money. But these three criteria exist in a state of conflict. Chemotherapy certainly doesn’t make us feel better. It often causes hair loss, nausea, rashes, low blood counts, and other unseemly side effects, sometimes for months or years at a time. But we accept chemotherapy’s toxicity in exchange for a chance at a longer life. Ditto the discomfort and inconvenience of surgery. And some therapies that make us feel better in the short term may also shorten our lives (though, paradoxically, some hospice services may actually prolong life).
Unfortunately, chemotherapy not only drains our energy level, but it is also likely to drain our bank account, and for modest life gains. New therapies for cancers often cost tens of thousands of dollars per month in exchange for an anticipated life prolongation of less than a year. That extra year may be precious, and I don’t mean to minimize it. But the cost adds up. For a drug costing ~$14,000 per month, a patient may have a copayment of ~$3,000 or more per month. Patients on Medicare, our national socialized medicine for elders, who are newly diagnosed with cancer incur out-of-pocket spending averaging 23.7 percent of their household income. Ten percent of Medicare folks with cancer have out-of-pocket spending equivalent to almost two-thirds of their household income. And for those of us not on Medicare, 40% of whom would not be able to find $400 in cash in an emergency, the cost is likely completely out of reach. So it’s no surprise that medical bankruptcy accounts for almost two-thirds of all U.S. family bankruptcy filings or that patients with cancer are 2.5 times as likely as non-cancer patients to file for bankruptcy.
For many patients, this financial toxicity is as feared as the physical toxicity of the drugs themselves. One of my physician colleagues darkly refers to the medical-industrial complex as being in the business of “farming sick people for money.” Elements of cancer care seem to confirm his suspicions. Financial toxicity is a big enough problem that the National Cancer Institute devotes a section of its website to helping patients navigate it.
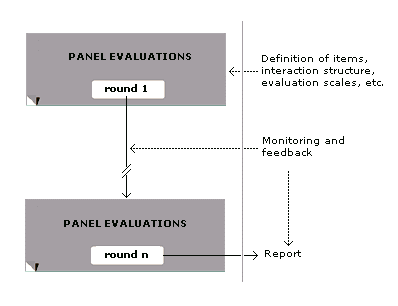
We shouldn’t just care about the topic because of our humanitarian impulses. We should care about its second-order effects. Financial distress, or even the fear of it, is associated with delayed initiation of treatment, limited patient adherence to treatment, and abandonment of recommended treatment. This is horrifying, and it’s not limited to cancer care. Here’s a model of how it might play out in heart disease, where financial toxicity has similarly been linked to poor outcomes:
Many are calling for greater adoption of the Center for Medicare and Medicaid Innovation’s Oncology Care Model, which identifies care navigation and connection of patients to resources as core functions of medical practice. But in spite of research demonstrating clear value, not every practice has a care navigator because of the lack of a sustainable model for reimbursement.
A potential strategy that may meet the Oncology Care Model halfway is the use of “community health workers,” laypersons with an intimate knowledge of specific populations that may be served by a practice. If a doctor has a hard time connecting with recent Vietnamese immigrants in her practice, for example, a Vietnamese-speaking CHW who has knowledge of the religion and culture of the region from which the patients immigrated may be able to work with them on shared decision-making around things like transportation, diet, adherence to medications, and even end-of-life planning.
[disclosure: the Kansas Business Group on Health has CDC funding related to increased adoption of community health workers]
Does your employee policy cover care navigation, or do you have personal experience with a community health worker? If so, we’d love to hear about it. If not, we’d love to help.
As the Medical Director of the Kansas Business Group on Health, I’m sometimes asked to weigh in on hot topics that might affect employers or employees. This is a reprint of a blog post from KBGH.