First, a story about the last time I cried: a few weeks ago, I began to wonder how Dr. Susan Braithwaite, one of my professors from my endocrine fellowship at the University of North Carolina, was doing. I had asked her for a letter of reference in January of this year, 2022, because I was applying for a part-time job back at my medical school alma mater, the University of Kansas School of Medicine here in Wichita.
I emailed her to ask for the letter, which seems kind of strange and unprofessional except for the fact that she was a furious, enthusiastic emailer; during hospital rounds, she would go from floor to floor, opening computers and buzzing through her inbox to make sure no patient or physician had contacted her with critical information in the last fifteen minutes. In her immediate emailed response to my request, she mentioned she was having some health issues, but that she hoped to get back to work soon. She graciously agreed to write my letter of reference. It was promptly delivered to the Promotion and Tenure Committee at KUSM-W.
I got the job, and I wrote her an e-mail to thank her for her help. I offered to send her a physical, snail-mailed thank-you note, but I didn't know her physical address, and I don't think she was interested in giving it to me. In my thank-you email, I mentioned that I had used, and continue to use, her basal-bolus insulin titration algorithm that she, with an alliterative panache, published as “Five Steps to Freedom” on New Year’s Day in 2005. If you’re curious, here are the five steps:
But I’m getting ahead of myself. I promised a story about crying, not a story about blood sugars. A few weeks ago, after using the Five Steps algorithm for what must have been my 1,000th patient, I wondered how her health was holding up. So, I sent her a quick email.
I did not get an immediate response.
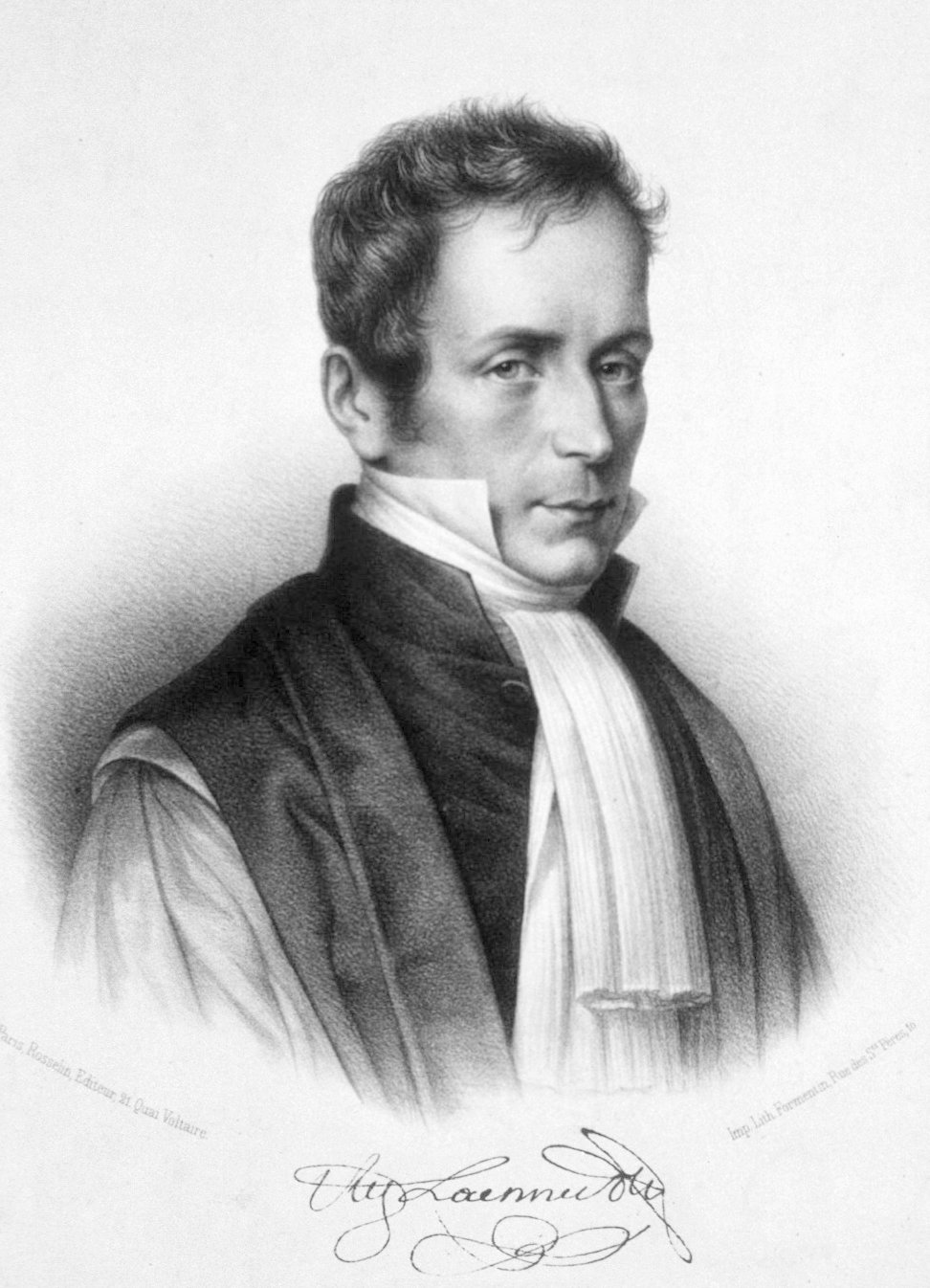
After a few days, I got a gmail nudge telling me that I had sent the email to Dr. Braithwaite five days earlier and asking, did I want to try again? I felt a wet, furry sense of dread. Instead of sending another email, I instinctively typed “Susan Braithwaite obituary” into Google and closed my eyes as I hit “enter.” Then I saw this:
And that’s when I cried. I cried for the reasons most of us cry when we encounter loss. I mostly cried for my guilt. I hadn’t reached out to her in January because I wanted to see how she was doing; I knew she’d taken a new job at Florida State, and I wasn’t curious enough to simply see how that was going for her. Nope. I reached out to ask a favor. And she gave it to me, even though she had maybe five months to live. It wasn’t even her first time doing me a favor. Once upon a time, she invited me to publish a letter with her in JAMA Internal Medicine, something I was underqualified to do. But she dragged me along, anyway, just like she helped hoist me into a new job at KUSM-W.
I also cried for the loss of such a beautiful, mathematical mind so dedicated to making the world a better place. But, in processing her loss, I thought of how many people will continue to benefit from her brief presence on Earth. She seemed to know her time was short, from the first moment I met her in 2006. She wouldn't talk to drug reps, a practice that I admired and now follow myself. I don’t think she saw them as a threat to her decision-making, the way some of us do. And there was no Sunshine Act back then, so she wasn’t protecting her reputation. I suspect she simply thought they were wasting her time. I wish I could say that she had endless time to spend with patients. Actually, I don’t. She didn’t have endless time to spend with patients. She had the exact amount of time it took to get an accurate history, do the proper exam, give advice, prescribe medications, and document the visit. She didn’t suffer through the rituals of the exam room that many of us believe make us better doctors. She refused, even, to type into the electronic health record. Instead, she would dictate a quick note in front of the patient, nodding to the patient to make sure she was getting the details right. Somehow (I really don’t know), the notes ended up in the EHR. They were shorter, more concise, and more useful than almost anyone else’s.
Instead, she spent her time using her mathematical mind to examine dose responses to insulin at varying blood glucose levels and coming up with novel treatment algorithms for critically ill patients with diabetes. I'm guilty of showing her graphs of insulin-versus-blood glucose levels in presentations of my own and intentionally breezing over them to hide my own mathematical shortcomings. And, though I can’t prove it, I suspect that modern-day smart insulin pumps use similar mathematical logic to what she was able to casually draw up on conference room whiteboards. To get a taste of this, see her 2014 paper on “Multiplicative standard deviation for blood glucose.” Or a dozen others. Just enter “Braithwaite SS” into Pubmed. You’ll find that her dozens of publications are pragmatic and aimed, laser-like, at the immediate, demonstrable improvement of patient care.
Sigh… my point is, Susan Shapiro Braithwaite lives on. She did the hard work of inching the science of medical delivery ever so slightly forward. And, for those of us in the academic world, that’s as close as we can get to immortality.