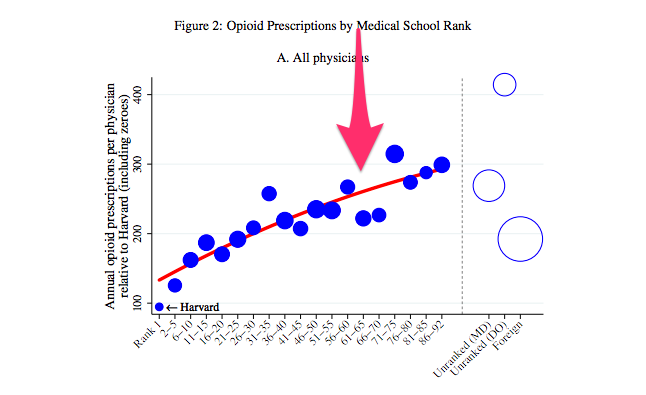
You read that headline right: investigators in an NBER paper found that docs who went to a lower US News-ranked school are more likely to write narcotic prescriptions, and the ones who write narcotic prescriptions are likely to write for more drugs, depending on the ranking of their school. And lordy, those osteopathic schools:
US News publishes several rankings, in topics from research to primary care to women's health. For this paper, the investigators used the "research" ranking, which is difficult to translate into medical student bedside education. After all, some of my best teachers in med school hadn't published a paper in a decade.
Several other take-home points from this. First, at first glance general practitioners write a ton of narcotic prescriptions; their rate on the y-axis is roughly double the overall physician population's. But when you consider that primary care docs perform well over half of all the visits delivered, that number of narc prescriptions looks less impressive.
Second, the effect size, if you're willing to take a leap and go straight to the idea that the quality of research at your medical school somehow has a causative effect on how many hydrocodone prescriptions you write, is huge. Using Harvard as the index school, the schools in the eighties and nineties have graduating docs writing three times as many prescriptions.
My first thought when I read this was that docs who went to lower-ranked schools may end up on places where they're more compelled to write narcotic prescriptions: places with high poverty, or a large blue-collar workforce, for instance. But the investigators accounted for that, and found that the relationship persisted even within the same county:
I can't help but try to apply this research to myself, even though I'm an endocrinologist and therefore mostly shielded from the narcotic game, and even though I see relatively few patients nowadays. But here we go. I attended the University of Kansas, which is comfortably ensconced in a tie at number 65 on the research list:
Oof. Medical school got a lot more expensive in the last couple decades.
So where would I live in the narc prescribing graph?
Riiiiiiiiight about there. It's a wonder I'm not a bonafide narcotic prescribing machine.
What's unsaid in this list is that KU has three campuses (two at the time of my training). And it further goes without saying that the training in Wichita, Salina, or Kansas City may have subtle differences that would lead to slightly different physician performance or behavior. Furthermore, it would be interesting to see the research repeated with residency or fellowship training as the independent variable, since those are the years when trainees really fall into a groove of prescribing habits. If I were held to the standard of my internship with a University of Washington program, I'd be compared to the folks at the skinny end of the graph:
Go dawgs.
But if my fellowship training at UNC-Chapel Hill were the standard, I'd be in a nice, comfortable happy medium between the narc-crazed sixties and the narc-stingy pre-teens:
The take-home from this isn't that we should all check our doctors' CVs before we go see them, in fear of them hooking us on oxycodone. It's just that schools who inhabit the lower tiers of medical research need to do a better job of teaching narcotic prescribing.
And obviously, the take-home for patients is to be very, very careful about requesting narcotics for pain. They don't work as well as we think they do, and the potential for harm is huge.
I found this link, fwiw, via marginalrevolution.com