If you’ve been to a Kansas Business Group on Health meeting in the last couple of years, you know already that American health care is beset by “low-value” care. We spend inordinate amounts of money doing “executive physicals” that offer almost no benefit. We pay for expensive back surgeries that are sometimes no better, and often worse, than physical therapy. We fail to substitute cheaper generic or bioequivalent drugs for more expensive drugs in spite of evidence that the less expensive drugs work just as well. All these low-value services account for between $75 billion and $100 billion in annual U.S. health care spending. In a $3.5 trillion health care economy, that seems like a rounding error. But it’s a big number! $100 billion is an extra $300 per year on health care per American.
What do most of these sins against our collective pocketbooks have in common? They mostly happen in specialist offices, not at the hands of primary care providers (PCPs). We’ve extolled the virtues of primary care often here at KBGH (although not necessarily the “annual check-up”). We’ve long known that primary care is the most cost-effective place to get your care. This was reinforced just last week in a new study looking at the sources of low value care.
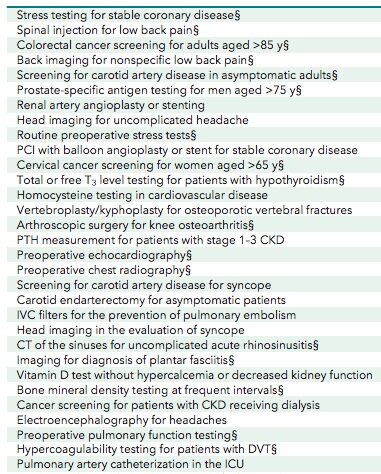
The investigators analyzed Medicare Part B claims from a 20% random sample of beneficiaries enrolled between 2007 and 2014. They excluded anyone in a given year who could not be linked to a PCP in the data, and they defined “low value services” as 31 services by various clinical guidelines:
Annals of Internal Medicine
When they looked at who ordered the low-value services, they found that PCPs accounted for a tiny fraction, 14.5%. But since many of the services you see above are not routinely done by PCPs, they looked further and found another 19.8% were performed or ordered by doctors to whom the patient was referred by the PCP, and another 5.6% was done by physicians to whom the patient had been referred by the PCP in the past.
The remaining 60.2% of low-value spending was “for services performed or ordered by a physician to whom the PCP never referred the beneficiary.” That is, almost two-thirds of the low-value spending was by physicians the PCP likely didn’t even know the patient was seeing! It’s possible the patient Googled “chest pain,” or answered a billboard for another service. The data doesn’t say.
This hurts me as a specialist physician. I wonder how many of the 31 low-value care items I’ve over-utilized in my career. Several of the items on the list, from certain thyroid tests to tests of vitamin D and parathyroid hormone, were right down my alley as an endocrine specialist. If it matters, the worst-offending non-primary care specialties for low-value spending were cardiology (27.3%), ambulatory surgical centers (8.9%), internal medicine (7.0%), orthopedic surgery (4.9%), and gastroenterology (4.8%). No endocrinology on that list. Whew!
All this isn’t to say that people don’t benefit from seeing more than one doctor. We’ve reviewed the myriad benefits of second opinions in past posts. But I do think that it reinforces the need for all of us to have a primary care physician directing our care. More than 84 percent of Americans have had contact with a health care professional in the past year, but only about half of those visits were to primary care offices, and only 75% of Americans have a primary care physician, a number that is declining over time.
None of us want to be accused of erecting barriers to good care. But I believe that adopting policies that encourage the use of primary care over, or ahead of, other services will be good for both the health of your employees and the bottom line of your company.
As the Medical Director of the Kansas Business Group on Health I’m sometimes asked to weigh in on hot topics that might affect employers or employees. This is a reprint of a blog post from KBGH.